What is Potassium?
Potassium is a chemical element with the symbol K (from Neo-Latin kalium) and atomic number 19. It is considered an alkali metal with a single electron in its outer shell, which is easily removed to create an ion with a positive charge.
Potassium ions are vital for the functioning of all living cells. To understand its importance, here’s a brief primer on sodium, potassium, and water homeostasis (balance).
A Brief Primer on Sodium-Potassium/Water Homeostasis
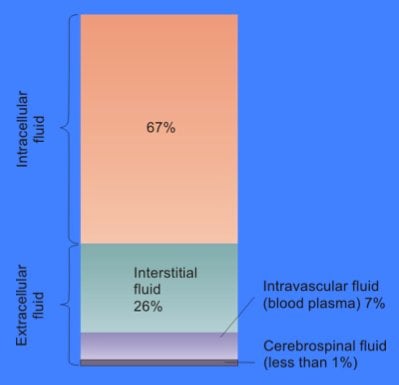
Water accounts for about ½ to ⅔ of an average person’s weight. For a 70-kg (154-lb) man, this means about 42 liters (10.5 gal) of water. Two-thirds of this water is inside the cells that make up our bodies and is referred to as intracellular fluid (ICF).
The rest is called extracellular fluid (ECF) and consists of the fluid between individual cells, plasma in the blood stream, and cerebrospinal fluid (the fluid that surrounds the brain and spinal cord).
The content of the ICF is very different than that of the ECF. ICF is high in potassium (140 mEq/l) compared to extracellular fluid (3.5-5 mEq/l)—nearly thirty times higher! On the other hand, the amount of sodium (chemical symbol Na) inside the cells (12 mEq/l) is very low compared to outside the cells (140 mEq/l).
Cell membranes, the covering of a cell that separates its contents from the extracellular space, are somewhat porous, meaning that small molecules and water can pass through.
The natural tendency, if there is a difference in the amount of a substance on either side of a membrane, is that water will pass through the membrane to equilibrate the concentration on both sides.
However, this difference in Na-K concentrations is so important that each cell has a sodium-potassium pump to actively pump Na out and K into cells to maintain the imbalance.
The sodium-potassium pump is integral to maintaining the body’s acid-base balance as well as kidney function. It also functions to maintain the electrical charge within a cell. This is vital to muscle and nerve cells, allowing for nerve transmission and muscle contraction.
Body fluid volume and electrolyte concentrations are maintained under normal conditions within very tightly controlled limits, despite large fluctuations in dietary intake, metabolic activity, and environmental stresses. Water and sodium balance are closely interdependent. In addition, the kidneys play a major role in maintaining the homeostasis of body fluids.
Now back to Potassium….
Potassium is present in many food items, in a wide variety of plant and animal foods and in beverages. Many fruits and vegetables are excellent sources, as are some legumes (e.g., soybeans) and potatoes.
Meats, poultry, fish, milk, yogurt, and nuts also contain potassium. [1] Among starchy foods, whole-wheat flour and brown rice are much higher in potassium than their refined counterparts, white wheat flour and white rice.
A study by O’Neil et al [2] the top sources of potassium in adults in the US are
- Milk
- Coffee, tea, other nonalcoholic drinks
- Potatoes
- Tomatoes, tomato/vegetable juice
- Fruit
- Beef
The forms of potassium in fruits and vegetables include potassium phosphate, sulfate, citrate, and others. In dietary supplements, potassium is often present as potassium chloride, but many other forms—including potassium citrate, phosphate, aspartate, bicarbonate, and gluconate—are also used.
The U.S. Department of Agriculture’s Nutrient Database lists the nutrient content of many foods and provides a comprehensive list of foods containing potassium, ordered by food name and by nutrient content. The 2015–2020 Dietary Guidelines for Americans provide a list of foods with at least 5% of the daily value for potassium per serving.
Potassium is absorbed via passive diffusion, primarily in the small intestine. It is estimated that the body absorbs about 85%–90% of dietary potassium, and it is used to maintain its normal intracellular and extracellular concentrations. Potassium is excreted primarily in the urine, although some is excreted in the stool, and a very small amount is lost in sweat.
The kidneys control potassium excretion in response to changes in dietary intakes. Potassium excretion increases rapidly in healthy people after potassium consumption, unless body stores are depleted. The kidneys can adapt to variable potassium intakes in healthy individuals, but a minimum of 5 mmol (about 195 mg) potassium is excreted daily in urine [1].
This, combined with other obligatory losses, suggests that potassium balance cannot be achieved with intakes less than about 400–800 mg/day [3].
According to the NIH Office of Dietary Supplements, the recommended adequate intakes for potassium by age, sex and additional condition are:
| Table 1: Adequate Intakes (AIs) for Potassium* | ||||
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months | 400 mg | 400 mg | ||
| 7–12 months | 700 mg | 700 mg | ||
| 1–3 years | 3,000 mg | 3,000 mg | ||
| 4–8 years | 3,800 mg | 3,800 mg | ||
| 9–13 years | 4,500 mg | 4,500 mg | ||
| 14–18 years | 4,700 mg | 4,700 mg | 4,700 mg | 5,100 mg |
| 19–50 years | 4,700 mg | 4,700 mg | 4,700 mg | 5,100 mg |
| 51+ years | 4,700 mg | 4,700 mg | ||
Until recently, humans consumed a diet high in potassium. However, increased use of processed foods, which typically remove potassium, and decreases in fruit and vegetable consumption have led to a decrease in daily potassium intake.
Dietary surveys consistently show that people in the United States consume substantially less potassium than recommended, which is why the 2015–2020 Dietary Guidelines for Americans identified potassium as a “nutrient of public health concern.”
According to data from the 2013–2014 National Health and Nutrition Examination Survey (NHANES), the average daily potassium intake from foods is 2,423 mg for males aged 2–19, and 1,888 mg for females aged 2–19. In adults aged 20 and over, the average daily potassium intake from foods is 3,016 mg for men and 2,320 mg for women.
Because of potassium’s wide-ranging roles in the body, low intakes can increase the risk of illness. Potassium intake deficiency can increase blood pressure, kidney stone risk, bone turnover, urinary calcium excretion, and salt sensitivity (meaning that changes in sodium intakes affect blood pressure to a greater than normal extent) [4].
Severe potassium deficiency can cause hypokalemia, (blood potassium level less than about 3.6 mmol/L). Mild hypokalemia is characterized by constipation, fatigue, muscle weakness, and malaise.
Moderate to severe hypokalemia (serum potassium level less than about 2.5 mmol/L) can cause polyuria (large volume of dilute urine); encephalopathy (brain disease, damage, or malfunction) in patients with kidney disease; glucose intolerance; muscular paralysis; poor respiration; and cardiac arrhythmias, especially in individuals with underlying heart disease.
Severe hypokalemia can be life-threatening because of its effects on muscle contraction and, therefore, cardiac function. [3]
Potassium supplements are available as pills or an oral solution. Because of the risk of excess potassium (see below) the FDA limits over-the-counter potassium supplements (including multivitamin-mineral pills) to less than 99 mg (which is only about 3% of the recommended daily value).
Is There any Research?
A review of PubMed reveals 1383 studies found using the term “potassium supplements.” Of these, 188 are review articles, and 210 are typed as “clinical trials.” ClinicalTrials.gov has only one completed clinical trial with potassium supplementation.
In comparison to another popular supplement, there are 84,904 scholarly publications related to Iron which includes almost 5000 human clinical trials.
Do Potassium Supplements Help Regulate Fluid Balance? (Water Retention)
Osmolality is a measurement of the total number of solutes in a liquid solution and is expressed in osmoles of solute particles per kilogram of solvent. In the case of body fluids, the main solutes we are talking about are electrolytes- sodium and potassium, glucose and urea.
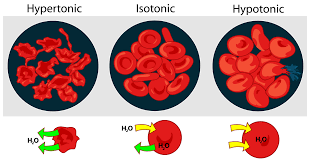
If there are electrolyte imbalances (and therefore osmolality differences) between the ICF and ECF, water flows from the side with lower osmolality to the side with higher osmolality to equalize it. This can cause cells to shrink or swell unless the body uses a combination of mechanisms to restore balance.
These mechanisms include:
- thirst to increase water intake
- pituitary hormones, such as vasopressin (also called antidiuretic hormone or ADH) to increase or decrease the amount of water reabsorbed by the kidneys
- osmosis- where water flows passively from one area or compartment of the body to another. For example, larger volumes of ECF can act as a reservoir for the smaller amount of fluid in blood vessels during a period of dehydration.
Based on all I’ve written so far, it’s fair to say that potassium has a role in the regulation of fluid balance. But, the mechanisms above can, for the most part, adjust for day to day changes in water availability. Adding additional potassium in the form of a pill is not going to make any noticeable changes in your body, unless of course, you are in a severe potassium deficit situation.
Bottom Line
Although potassium is an important component of fluid balance, potassium supplements are usually not necessary to maintain fluid balance.
Do Potassium Supplements Help Reduce Blood Pressure?
Based on potassium’s important role in sodium and water homeostasis, it would not be surprising to say that potassium plays a role in maintaining blood pressure (BP). Epidemiologic, experimental and clinical studies have found potassium to be an important regulator of blood pressure. Potassium depletion has been found to increase the risk of high BP, especially when combined with high sodium intake.
The mechanism is not totally understood, but sodium retention, altered response to vasoactive hormones (which affect the diameter of blood vessels), direct vasoconstrictive effects of hypokalemia, and calcium depletion may all contribute to the blood pressure elevation during potassium depletion.[5]
Epidemiologic studies from divergent geographic locations have found that populations with lower potassium intakes have higher incidences of hypertension. A large international collaboration [6] with over 10,000 subjects in 52 centers correlated 24-hour urine electrolyte excretion with blood pressure.
BP rose with increased sodium intake and lowered with increases in potassium intake. It should be noted, however, that these epidemiologic correlations do not prove a causal relationship- something other nutrient(s) could be involved in this observation.
Experiments in rats [7, 8] showed that severe potassium depletion stunts growth and lowers BP. Linas et al [9, 10] also found decreases in BP with potassium depletion in rats with normal BP and in rats made hypertensive by clipping one renal artery. They attribute the decrease to lower peripheral vascular resistance and impaired response to angiotensin II (a hormone that causes vasoconstriction and an increase in BP).
Krishna et al [11] [5, 12] did several clinical studies looking at the effect of potassium depletion on blood pressure in both normotensive and hypertensive human subjects. Their studies demonstrated that short-term potassium depletion increases both systolic and diastolic blood pressure in normotensive and hypertensive patients on normal sodium diets but not in patients on a low sodium diet.
What effect can potassium supplements play in decreasing blood pressure? Two systematic reviews and meta-analyses look at this issue. The first, by Aburto et al [13], looked at 21 randomized controlled trials in adults.
They confirmed that increasing potassium intake reduces systolic and diastolic BP. However, the results vary somewhat depending on the population included. Some studies only had patients with hypertension, while others had both hyper- and normotensive subjects.
Three studies with only normotensive subjects showed no detectable effect of potassium supplement on BP. When the authors try to minimize the role heterogeneity plays by eliminating some studies, they conclude that “Increased potassium intake reduced systolic blood pressure by 3.49 (1.82 to 5.15) mm Hg and diastolic BP by 1.96 (0.86 to 3.06) mm Hg.” Not a huge amount!
The second, by Filippini et al [14], included 25 studies (1163 subjects) of greater than 4 weeks duration and where urinary sodium and potassium values were available. They found that potassium supplementation had a significant BP-lowering effect, which emerged in studies at 8-12 weeks.
Their results suggested that “long-term ‘moderate’ supplementation with potassium salts can reduce BP in hypertensives, and that such effect may be particularly relevant in individuals not on drug treatment, having a high sodium intake, and characterized by a baseline potassium intake < 90 mmol/day.”
Bottom line
Potassium levels play a significant role in blood pressure control. Low potassium levels are associated with increased BP. Potassium supplementation can decrease blood pressure however how significant a decrease is unclear due to study heterogeneity. Increasing potassium through dietary intervention is probably the safest way to supplement potassium.
Do Potassium Supplements Help Protect Against Strokes?
As potassium plays a role in blood pressure control, it’s probably not surprising that potassium has been examined as a means of reducing the risk of stroke. As to whether potassium can reduce the risk of stroke in ways other than blood pressure regulation will also be discussed.
In addition to the effect of potassium on blood pressure, the meta-analysis by Aburto et al [13] (above) examined the effect on stroke risk. An analysis of 9 cohorts detected a protective effect of higher potassium intake on the risk of stroke, especially when the potassium intake was <90mmol/day.
D’Elia et al [15] did a meta-analysis of 11 studies which included almost 250,00 participants between 1971 and 2000. In this group, there were 7066 strokes, 3058 coronary heart disease events and 2497 coronary vascular events. In their pooled analysis, they found that a 42 mmol/day (1640 mg) higher potassium take was associated with a 21% lower risk of stroke.
However, there are two potential problems with the study. One is that they do not factor out how much of the effect is due to a lowering of blood pressure. Secondly, the studies involved measure potassium intake in different ways: 24-h dietary recall (n = 2), food frequency questionnaire (n = 6), or 24-h urinary excretion (n = 3).
The first two methods can be rather subjective and less reliable.
A more recent meta-analysis by Vinceti et al [16] examined 16 cohort studies, and compared the relative risk (RR) of stroke between individuals in the lowest potassium intake groups with those with highest potassium intake. They confirmed the inverse association between potassium intake and stroke risk.
Potassium intake of 90 mmol (≈3500 mg)/day was associated with the lowest risk of stroke. They also analyzed the data with and without adjusting BP. The effect on RR was still present but was not as great when BP was factored out. Like D’Elia, they point out that some of their data relied on less-reliable methods to assess potassium intake, such as those where potassium is calculated based the on concentration in spot urine samples vs. 24-hr urine collections.
They also could not rule out the degree that other coexisting minerals or dietary variables could play in their results.
He et al [17] tried to assess what additional mechanisms (other than BP) can explain the decreased risk of stroke with higher potassium intake. They performed a randomized, double-blind crossover trial on 42 subjects who were given either potassium bicarbonate, potassium chloride or placebo capsules daily for 4 weeks.
They found that compared with placebo, both potassium chloride and potassium bicarbonate significantly improved endothelial function (measured by brachial artery flow-mediated dilatation), increased arterial compliance (assessed by carotid-femoral pulse wave velocity), decreased left ventricular mass, and improved left ventricular diastolic function.
The FDA has approved the following health claim: “Diets containing foods that are a good source of potassium and that are low in sodium may reduce the risk of high blood pressure and stroke.”
Bottom Line
Potassium intake plays a role in the prevention of stroke both through a decrease in blood pressure as well as effects on the vasculature (blood vessels) and heart. The amount necessary to decrease risk varies somewhat from study to study and may be partially due to variations in how potassium intake was measured.
Do Potassium Supplements Help Prevent Kidney Stones?
Kidney stones are most common in people aged 40 to 60. Stones containing calcium—in the form of calcium oxalate or calcium phosphate—are the most common type of kidney stone.
Low potassium intakes impair calcium reabsorption within the kidney, increasing urinary calcium excretion and potentially causing hypercalciuria (high calcium in the urine) and kidney stones. Low urinary levels of citrate also contribute to kidney stone development. [3]
An observational study by Curhan et al [18], looking at a group of over 45,000 men aged 40-75 with no previous history of kidney stones, found those with the highest potassium intakes (≥4,042 mg/day on average) had a 51% lower risk of kidney stones over 4 years of follow-up than those with the lowest intakes (≤2,895 mg/day).
Curhan did a similar study in a group of over 90,000 women [19] and found that those who with a daily potassium consumption of over 4000 mg/day had a 35% lower risk of kidney stones.
A few studies have shown that potassium citrate can decrease the formation of calcium stones [20-22], but the citrate seems to be the more important component.
Bottom Line
Observational studies imply a higher potassium diet is protective in the formation of kidney stones. However direct double-blind, placebo-controlled studies are needed to define potassium’s role in prevention and treatment of kidney stones.
Do Potassium Supplements Help Prevent Osteoporosis?
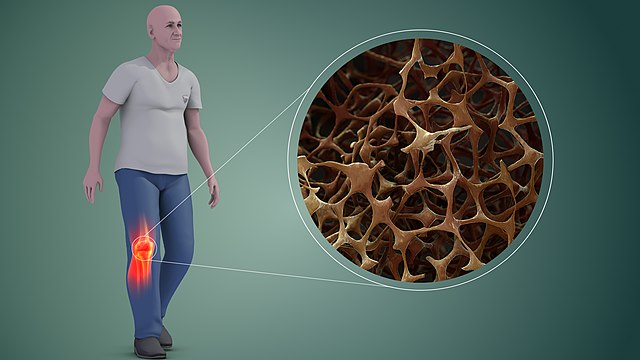
Osteoporosis, or porous bone, is a disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased risk of fractures of the hip, spine, and wrist.
Men as well as women are affected by osteoporosis, a disease that can be prevented and treated. In the United States, more than 53 million people either already have osteoporosis or are at high risk due to low bone mass. Worldwide, osteoporosis causes more than 8.9 million fractures annually, resulting in an osteoporotic fracture every 3 seconds. [23]
Many have speculated that a modern Western diet, low in fruit in vegetables and high in starch is a high acid-generating diet which leads to a low-grade metabolic acidosis. In order to buffer the excess acid, the body “reaches into” the large reservoir of alkaline calcium salts in the bone, thereby deleting bone calcium.
Can alkaline components in the form of potassium salts (potassium bicarbonate or citrate), either from food or potassium supplements counter this effect and help preserve bone tissue?
Observational studies suggest that increased consumption of potassium from fruits and vegetables is associated with increased bone mineral density [24]. In the Framingham Heart Study, for example, higher potassium intake was associated with significantly greater bone mineral density in 628 elderly men and women [25].
In another study [26], the National Heart, Lung and Blood Institute’s DASH diet significantly reduced biochemical markers of bone turnover. However, because the DASH eating pattern has a lower acid load than typical Western diets, and is also high in calcium and magnesium in addition to potassium, it is difficult to determine any independent contribution of potassium.
Only a few clinical trials have examined the effects of potassium supplements on markers of bone health. He’s study [17] on the effects of potassium on cardiovascular risk also examined signs of bone turnover. Subjects given potassium bicarbonate had significantly decreased 24-hour levels of urinary calcium and plasma βCTX, a marker of bone reabsorption.
In a double-blind, randomized, placebo-controlled study by Dawson-Hughes et al [27] 233 men and women, ages > 50 were given placebo or 1 or 1.5 mmol/kg/day potassium bicarbonate (KHCO3) for 3 months.
Compared to those given placebos, those given the lower dosage of KHCO3 had lower levels of urinary calcium, NTX (N-terminal telopeptide, a biomarker used to measure the rate of bone turnover), as well as serum P1NP (another biomarker of bone loss).
Jerle et al [28] enrolled 201 elderly (>65 yr old) healthy adults given placebo or potassium citrate daily (as well as calcium and Vit D to all) for 2 years. Treatment with potassium citrate resulted in a significant increase in bone density in lumbar spine and improved bone microarchitecture in the radius and tibia bones.
On the other hand, a study by Macdonald et al [29] looked at 276 postmenopausal women (ages 55-65) who were given either high or low-dose potassium citrate, 300 g addition fruit and vegetables/day (the equivalent of 18.5 mEq alkali), or a placebo for 2 years. They did not find any significant reduction of bone turnover, or increased bone density.
Finally, a 2015 meta-analysis of 16 studies by Lambert et al [30] examined the effect of potassium bicarbonate or potassium citrate on bone metabolism. They found that “urinary calcium excretion was lowered by intervention with both KHCO3 (P = 0.04) and KCitr (P = 0.01), as was net acid excretion (NAE) (P = 0.002 for KHCO3 and P = 0.0008 for KCitr).
Both salts significantly lowered the bone resorption marker NTX (P < 0.00001). There was no effect on bone formation markers or BMD. KHCO3 and KCitr lowered calcium excretion to a greater extent than did KCl.”
Bottom line
Overall, higher intakes of potassium from diets that emphasize fruits and vegetables, or potassium supplements with citrate or bicarbonate, might improve bone health. However, more research is needed to elucidate the underlying mechanisms and tease out potassium’s individual contribution.
Are Potassium Supplements Safe?
Potassium from food has not been shown to cause any harm in healthy people who have normal kidney function. Excess potassium is eliminated in the urine.
However, people who have chronic kidney disease and those who use certain medications can develop abnormally high levels of potassium in their blood (a condition called hyperkalemia). Examples of these medications are angiotensin converting enzyme inhibitors, also known as ACE inhibitors, and potassium-sparing diuretics.
Hyperkalemia can occur in these people even when they consume typical amounts of potassium from food.
Hyperkalemia can also develop in people with type 1 diabetes, congestive heart failure, liver disease, or adrenal insufficiency. Adrenal insufficiency is a condition in which the adrenal glands, located just above the kidneys, don’t produce enough of certain hormones.
Even in healthy people, getting too much potassium from supplements or salt substitutes can cause hyperkalemia if they consume so much potassium that their bodies can’t eliminate the excess.
Although hyperkalemia can be asymptomatic, severe cases can cause muscle weakness, paralysis, heart palpitations, paresthesias (a burning or prickling sensation in the extremities), and cardiac arrhythmias that could be life-threatening.
Some medications can interact with potassium, and include:
- ACE inhibitors and angiotensin receptor blockers (ARBs)
ACE inhibitors, such as benazepril (Lotensin®), and ARBs, such as losartan (Cozaar®), are used to treat high blood pressure, heart disease, and kidney disease. They decrease the amount of potassium lost in the urine and can make potassium levels too high, especially in people who have kidney problems. - Potassium-sparing diuretics
Potassium-sparing diuretics, such as amiloride (Midamor®) and spironolactone (Aldactone®), are used to treat high blood pressure and congestive heart failure. These medications decrease the amount of potassium lost in the urine and can make potassium levels too high, especially in people who have kidney problems. - Loop and thiazide diuretics
Loop diuretics, such as furosemide (Lasix®) and bumetanide (Bumex®), and thiazide diuretics, such as chlorothiazide (Diuril®) and metolazone (Zaroxolyn®), are used to treat high blood pressure and edema. These medications increase the amount of potassium lost in the urine and can cause abnormally low levels of potassium.
Tell your doctor, pharmacist, and other healthcare providers about any dietary supplements and prescription or over-the-counter medicines you take. They can tell you if the dietary supplements might interact with your medicines or if the medicines might interfere with how your body absorbs, uses, or breaks down nutrients, such as potassium.
Conclusion
Potassium is an essential element in the proper functioning of our bodies. It plays key roles in sodium and fluid balance, acid/base balance, nerve transmission, and heart and muscle function.
The federal government’s 2015–2020 Dietary Guidelines for Americans notes that “Nutritional needs should be met primarily from foods. … Foods in nutrient-dense forms contain essential vitamins and minerals and also dietary fiber and other naturally occurring substances that may have positive health effects.”
Dietary sources of potassium include fruits and vegetables, milk, seafood, lean meats, poultry, legumes (beans and peas), nuts, seeds (like Chia) and soy products. Believe it or not, the potato is the highest source of potassium of all foods (738 mg in a standard portion)! Topping it with yogurt adds another 530-580 mg of potassium.
If you want to add supplemental potassium, please check with your healthcare provider before beginning, especially if you have one of the risk factors mentioned above.

Leave a Reply